NSP: Tool Components and Descriptions (2018)
Screening Tools for Identifying Risk for Malnutrition in the Pediatric PopulationDownload a copy of the Components Table (PDF)
Table. Pediatric Nutrition Screening Tool Components
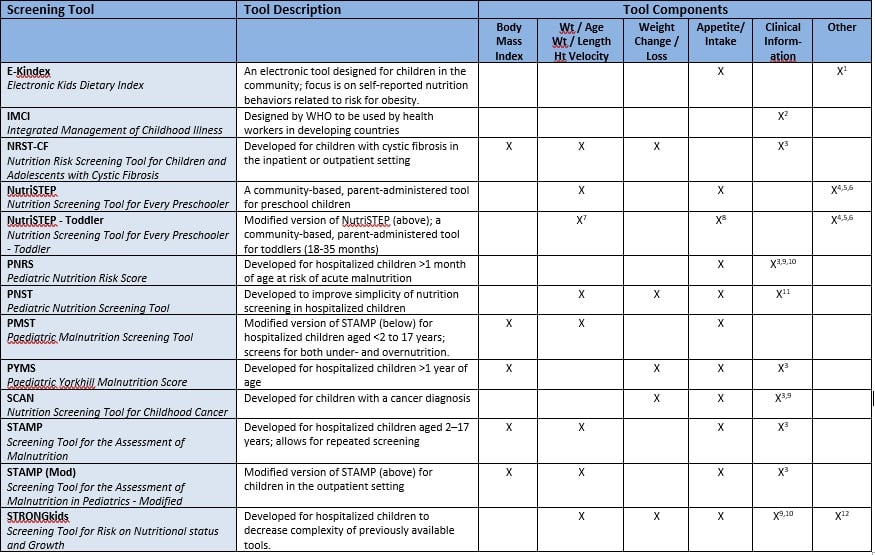
1Dietary habits, cooking techniques, meal patterns
2Visible severe wasting, bipedal edema
3Medical condition or diagnosis, severity of disease or intensive treatment which may affect nutritional intake
4Dietary behavior
5Physical activity/sedentary behavior
6Food security; screen time
7Includes parent/caregiver reported concerns about weight/growth
8Includes parent/caregiver reported concerns about oral and feeding skills
9Gastrointestinal symptoms causing nutritional losses (vomiting, diarrhea)
10Pain or other symptoms causing inability to eat
11Visibly under-overweight
12Pre-existing nutrition intervention
Tool Descriptions
Electronic Kids Dietary Index (E-Kindex) was developed by researchers at the Harokopio University, Department of Nutrition-Dietetics, Athens, GREECE and the University of Cyprus, Department of Psychology, Nicosia, CYPRUS. It is an electronic screen for unhealthy dietary behaviors that relates to the development of obesity in children. It includes factors from 3 areas: Part 1, Foods: E-KINDEX relates to food items and cooking techniques. Part 2, Behavior: E-KINDEX relates to dietary attitudes and related behavior. Part 3: E-KINDEX related to dietary habits evaluates meal patterns and behavior. A resulting 4-point scoring system (0 to 3 or the reverse) was used (Lazarou et al, 2011).
Nutrition Risk Screening Tool for Children and Adolescents with CF (NRST-CF) developed by McDonald as a screening tool that is a risk-based classification system with 3 categories: weight gain, height velocity, and body mass index. The tool incorporates the CF Foundation Recommendations risk points assigned when minimum body mass index, weight gain, and/or height gain standards are unmet. The tool adds defined clinical variables which promotes earlier identification of nutritional risk in pediatric patients with CF. (McDonald, 2008).
Nutrition Screening Tool for Every Preschooler (NutriSTEP) was developed by dietitians in Canada to determine the nutrition risk of the general preschool population. It is a community-based, parent-administered screening tool available in English, French, Traditional Chinese, Simplified Chinese, Punjabi, Spanish, Tamil, and Vietnamese. It is available in paper, internet, or onscreen format. The tool consists of 17 items with five questions focused on food group intake and the remaining 12 cover physical growth, food and fluid intake, physical activity and sedentary behavior and factors affecting food intake for preschoolers. Each item has a minimum score of 0 (no risk) and maximum score of 4 (risk). The item responses are summed to a maximum score of 68. An increase in score indicates an increased nutrition risk (Carducci et al, 2015).
After the Nutrition Screening Tool for Every Preschooler (NutriSTEP) was developed by dietitians in Canada and released in 2008, it was identified that a screening tool was needed for toddlers. In 2012, the Toddler NutriSTEP was released to identify nutrition issues in children ages 18-35 months. It is a community-based, parent-administered screening tool available in English, Spanish and French. The tool consists of 17 items with six questions focused on food and beverage intake and the remaining 11 cover physical growth, physical activity and psychosocial factors including toddler specific eating behaviors food security. Each question is scored from 0 to 4 with a maximum score of 68. Nutrition risk is based on the score with a higher score indicating an increased nutrition risk (Randall Simpson et al, 2015).
Pediatric Nutrition Risk Score (PNRS) was developed to screen pediatric inpatients greater than 1 month old at risk of acute malnutrition. Nutrition risk factors were evaluated within 48 hours of admission to screen for nutrition risk and can be administered by nursing or medical staff. Risk factors include food intake and ability to eat, ability to retain food due to vomiting and diarrhea, pain or other symptoms that interfere with food intake, severity of disease and anthropometrics. The score is from 0 to 5 and with 0 points indicating low nutrition risk 1-2 points indicating moderate nutrition risk and 3-5 points indicating high nutrition risk (Sermet-Gaudelus et al, 2000).
Pediatric Nutrition Screening Tool (PNST) was developed by a group of Australian dietitians and nurses in 2016 looking to improve simplicity in nutrition screening tools in order to improve use in hospitalized pediatric patients. Developers of PNST focused on avoiding the necessity of additional tables for high nutrition related risk diseases or pathological conditions and the requirement to obtain anthropometric data for risk stratification. PNST consists of 4 simple yes/no questions (weight loss, poor weight gain, decreased intake, visibly under/overweight) whereby 2 affirmative responses are used as a predictor of nutrition risk (White et al, 2016).
Paediatric Malnutrition Screening Tool (PMST) is a modified version of the Screening Tool for the Assessment of Malnutrition in Paediatrics (STAMP) developed for hospitalized children. The PMST includes children less than 2 years of age up to 17 years of age and the same three components used in the STAMP: clinical diagnosis, estimated nutritional intake, and weight and height percentiles. Each component carries a score of 1-3 and the total score reflects the risk of undernutrition and overnutrition. The clinical diagnosis component for PMST includes additional malnutrition risk points for overweight (BMI>85th percentile) and obesity (BMI>98th percentile). An overall score of 2 or 3 indicates medium risk and a score ≥ 4 indicates high risk (Thomas et al, 2016).
Paediatric Yorkhill Malnutrition Score (PYMS) was developed for use at the Royal Hospital for Sick Children (RHSC), Yorkhill, Glasgow. The criteria was based on the guidelines of the European Society of Clinical Nutrition and Metabolism for nutritional screening. The PYMS assesses four steps, all recognised predictors or symptoms of malnutrition: BMI, history of recent weight loss, changes in nutritional intake, and the predicted effect of the current medical condition on the nutritional status of the patient, with questions and points for each step, resulting in a sum total indicating a category of malnutrition risk of mild, moderate or severe. Each step bears a score of up to 2 and the total score reflects the degree of the nutrition risk of the patient. A score of 1 indicates medium risk and 2 or above, high risk (Gerasimidis et al, 2010; Wonoputri et al, 2014)
Nutrition Screening tool for Childhood Cancer (SCAN) was developed by an interdisciplinary team at the Children’s Nutrition Research Center Queensland Children’s Medical Research Institute University of Queensland Brisbane Australia in 2014. The tool was developed to identify children with a diagnosis of cancer for risk of malnutrition. The tool consists of 6 questions with scoring determined by clinical evaluation of each criteria’s contribution to nutrition risk. Each response is allocated a 1 or 2. A sum total of 3 or greater indicating risk of malnutrition. Questions include presence of high risk cancer, undergoing intensive treatment, presence of GI symptoms, weight loss, poor oral intake, signs of poor nutritional status (Murphy et al, 2016).
Screening Tool for the Assessment of Malnutrition (STAMP) in Pediatrics was developed in in the United Kingdom. It is a screening tool specifically developed for use in hospitalized children aged 2–17 and designed for use by members of a multidisciplinary team who have assessment training. STAMP incorporates three components: clinical diagnosis, estimated nutritional intake, and weight and height percentiles. Each component carries a score of 1-3 and the total score reflects the risk of undernutrition. A score of 2 or 3 indicates medium risk and a score ≥ 4 indicates high risk (McCarthy et al, 2012; Wong et al, 2013).
STRONGKIDS (Screening Tool for Risk on Nutritional status and Growth) was developed in the Netherlands in an attempt to decrease complexity of previously available tools. The STRONGkids tool is comprised of four areas: 1. Subjective clinical assessment (1 point), 2. High risk disease (2 points), 3. Nutritional intake and losses (1 point), and 4. Weight loss or poor weight gain (1 point). Risk levels are then assigned by point totals: 0 = low risk, 1-3 = medium risk, and 4-5 = high risk. STRONGkids also provides recommendations for nutritional intervention based on risk level whereby high risk includes recommendations for a nutrition evaluation by both physician and dietitian. (Hulst et al, 2009; Huysentruyt et al, 2013)
Screening Tool for the Assessment of Malnutrition in Pediatrics (STAMP)-modified is derived from a screening tool developed for use in hospitalized children that was modified for use outpatient clinics. The original STAMP three component scoring system: clinical diagnosis, estimated nutritional intake, and weight and height percentiles are preserved. Each component is scored from 1-3 with the total score reflecting the risk of undernutrition. The modification for outpatient use was to lower the scoring level since any deviation in a presumed healthy child indicates a nutrition risk. A score of 1 to 3 indicates medium risk and a score > 4 indicates high risk. (Rub et al, 2016)
Integrated Management of Childhood Illness (IMCI) was developed by WHO as an integrated management of childhood illness guidelines to help health-workers in first level facilities in developing countries to identify and manage sick children. Because length or height is not a usual measure in primary clinics primarily due to being time consuming and lack of accuracy, the IMCI relies on symptoms and clinical signs for screening. Health care workers identify extreme protein-calorie malnutrition by the presence of visible severe wasting and bipedal edema. (Hamer et al 2004)
REFERENCES
Carducci B, Reesor M, Haresign H, Rysdale L, Keller H, Beyers J, Paquette-Duhaime S, O'Connor A, Simpson JR. NutriSTEP® is Reliable for Internet and Onscreen Use. Can J Diet Pract Res. 2015 Mar;76(1):9-14. PMID: 26067241
Gerasimidis K, Keane O, Macleod I, Flynn D, Wright C. A four-stage evaluation of the Pediatric Yorkhill Malnutrition Score in a tertiary hospital and a district general hospital. BJ Nutr 2010; 104 751-756. doi: 10.1017/S0007114510001121. Epub 2010 Apr 19. PMID: 20398432.
Hamer C, Kvatum K, Jeffries D., Allen S. Detection of severe protein-energy malnutrition by nurses in The Gambia. Arch Dis Child. 2004; 89:181-184.
Hulst JM, Zwart H, Hop WC, Joosten KF. Dutch national survey to test the STRONGkids nutritional risk screening tool in hospitalized children. Clin Nutr. 2010 Feb;29(1):106-11. doi: 10.1016/j.clnu.2009.07.006. Epub 2009 Aug 13. PMID: 19682776
Huysentruyt K, Alliet P, Muyshont L, Rossignol R, Devreker T, Bontems P, Dejonckheere J, Vandenplas Y, De Schepper J. The STRONG(kids) nutritional screening tool in hospitalized children: a validation study. Nutrition. 2013;29(11-12):135-61. doi: 10.1016/j.nut.2013.05.008. PMID: 24103513
Lazarou C, Panagiotakos DB, Spanoudis G, Matalas AL. E-KINDEX: a dietary screening tool to assess children's obesogenic dietary habits. J Am Coll Nutr. 2011 Apr;30(2):100-12. PMID: 21730218
McCarthy H, Dixon M, Crabtree I, Eaton-Evans MJ, McNulty H. The development and evaluation of the Screening Tool for the Assessment of Malnutrition in Paediatrics (STAMP©) for use by healthcare staff. J Hum Nutr Diet. 2012 Aug;25(4):311-8. doi: 10.1111/j.1365-277X.2012.01234.x. Epub 2012 May 9. PMID: 22568534
McDonald CM. Validation of a nutrition risk screening tool for children and adolescents with cystic fibrosis ages 2-20 years. J Pediatr Gastroenterol Nutr. 2008 Apr;46(4):438-46. doi: 10.1097/MPG.0b013e318156c2db. PMID: 18367958.
Murphy AJ, White M, Viani K, Mosby TT. Evaluation of the nutrition screening tool for childhood cancer (SCAN). Clin Nutr. 2016 Feb;35(1):219-24. doi: 10.1016/j.clnu.2015.02.009. PMID: 25765336
Rub G,Marderfeld L,Poraz I,Hartman C,Amsel S,Rosenbaum I,Pergamentzev-Karpol S,Monsonego-Ornan E,Shamir R. Validation of a Nutritional Screening Tool for Ambulatory Use in Pediatrics. Journal of pediatric gastroenterology and nutrition 2016; 62:771-5.
Sermet-Gaudelus I, Poisson-Salomon AS, Colomb V, Brusset MC, Mosser F, Berrier F, Ricour C. Simple pediatric nutritional risk score to identify children at risk of malnutrition. Am J Clin Nutr. 2000 Jul;72(1):64-70. PMID: 10871562.
Randall Simpson J, Gumbley J, Whyte K, Lac J, Morra C, Rysdale L, Turfryer M, McGibbon K, Beyers J, Keller H. Development, reliability, and validity testing of Toddler NutriSTEP: a nutrition risk screening questionnaire for children 18-35 months of age.Appl Physiol Nutr Metab. 2015 Sep;40(9):877-86. doi: 10.1139/apnm-2015-0048. Epub 2015 Apr 30. PMID: 26300014
Thomas PC, Marino LV, Williams SA, Beattie RM. Outcome of nutritional screening in the acute paediatric setting. Arch Dis Child. 2016 Dec;101(12):1119-1124. doi: 10.1136/archdischild-2016-310484. Epub 2016 Sep 8. PMID: 27609019.
White M, Lawson K, Ramsey R, Dennis N, Hutchinson Z, Soh XY, Matsuyama M, Doolan A, Todd A, Elliott A, Bell K, Littlewood R. Simple Nutrition Screening Tool for Pediatric Inpatients. JPEN J Parenter Enteral Nutr. 2016 Mar;40(3):392-8. doi: 10.1177/0148607114544321. PMID: 25096546
Wong S, Graham A, Hirani SP, Grimble G, Forbes A. Validation of the Screening Tool for the Assessment of Malnutrition in Paediatrics (STAMP) in patients with spinal cord injuries (SCIs). Spinal Cord. 2013; 51:424-429. PMID 23295470
Wonoputri N, Djais J, Rosalina. Validation of Nutritional Screening Tools for Hospitalized Children. J Nutr Metab. 2014. doi. 10.1155/2014/143649